"Daddy - why are you here? I thought you were miles
away!"
"Well, I was," said Mr Rivers. "But Miss Grayling telephoned
to me to say that little Sally Hope had appendicitis and the surgeon they
usually had was ill, so could I come straight along and do the operation.
So of course I did! I hopped into the car, drove here, found everything
ready, did the little operation, and here I am! And Sally will be quite
all right and back again in school in about two weeks' time!"
. . . in the San, Sally slept . . . her pain gone . . . What a deft, quick
surgeon Darrell's father was - only thirteen minutes to do the operation!
Matron thought how lucky it was that he had been near enough to come.
(Enid Blyton, First Term at Malory Towers, Methuen & Co, 1946,
pp117, 119)
One thing which researchers need to bear in mind is that,
for disabled people, it is often impossible to separate our experiences
within the medical, social services and benefit systems (these latter are
also discussed here) from the rest of our daily lives. The combination
of our impairments and the effects of the medical![]() and administrative
and administrative![]() models of disability mean that this is inevitable. However, many people
within the disability movement would still say the fact that I am disabled
is what is relevant, rather than the nature of my impairment. But I have
included the following section for three reasons: to provide some insights
into the way in which disabled people, and disabled women in particular,
are treated by the British medical establishment (thus illustrating the
effects of the medical model of disability); to raise awareness of a potentially
disabling condition which can affect teenagers for the rest of their lives
and which is all too often overlooked or ignored by their parents, teachers
and doctors; and to provide a record of my individual experiences which
I will leave to others to analyse and to place within broader experiences
and histories of disability. What follows is a description of my personal
history of disablement within the medical system during the period covered
by my research, revealing the medical details of my impairment as I discovered
them myself.
models of disability mean that this is inevitable. However, many people
within the disability movement would still say the fact that I am disabled
is what is relevant, rather than the nature of my impairment. But I have
included the following section for three reasons: to provide some insights
into the way in which disabled people, and disabled women in particular,
are treated by the British medical establishment (thus illustrating the
effects of the medical model of disability); to raise awareness of a potentially
disabling condition which can affect teenagers for the rest of their lives
and which is all too often overlooked or ignored by their parents, teachers
and doctors; and to provide a record of my individual experiences which
I will leave to others to analyse and to place within broader experiences
and histories of disability. What follows is a description of my personal
history of disablement within the medical system during the period covered
by my research, revealing the medical details of my impairment as I discovered
them myself.
med1
I have always been disabled to some extent. I have probably
been visually impaired since birth, although this was not realised until
I was about seven or eight years old. In contrast to the 1990s, there was
very little awareness of sight problems among children in the 1960s, and
I was therefore one of only a few children in the school to wear spectacles.
At this time, spectacles were perceived purely in medical terms, so there
were only two styles available for children, neither of which had taken
aesthetic considerations into account. Wearing spectacles was a major factor
in my being bullied, and I was therefore disabled by my impairment to a
much greater extent than the many other visually impaired children within
the school whose sight remained uncorrected. The effect of the bullying
was also to make me do without spectacles wherever possible, impeding myself.
By the 1980s, though, many more people were recognised as being visually
impaired; spectacles came in a range of fashionable frames; and the disabling
factor had become negligible. The development of contact lenses also meant
that my impairment could be overcome to a much greater extent.
med2
I also suffered from a number of medical problems as a
child, which left my immune system weakened and as a teenager I suffered
from severe chicken pox followed by pneumonia and recurring chest problems,
as well as from numerous minor illnesses. I also suffered a fracture of
my right elbow following a fall at the age of fourteen, and a spontaneous
fracture of my right foot at the age of nineteen, which left both limbs
permanently weakened and put an end to my dancing career![]() .
.
med3
After beginning work as a journalist in 1984 at the age
of twenty-one, I began to suffer from severe migraines, but these were
eventually traced to an allergy to cows' milk products, and by cutting
these out of my diet the migraines ceased. (I am also allergic to eggs
and potatoes, although I enjoy sheep and goats' milk products and sweet
potatoes without any ill-effects.) Shortly after this, in autumn 1985,
after moving to the East End of London, I suffered from a chest infection
which took six months to shake off, but following this I enjoyed relatively
"good" health for four years. In September 1988, at the age of
twenty-six, I began my research into girls' school stories at the University
of East London, when I registered for a part-time M.A. by Independent Study.![]() At the same time, I continued to work as a freelance journalist
At the same time, I continued to work as a freelance journalist![]() ,
fitting in my studies around paid work. However, after I had been studying
for just over a year, in December 1989, I developed another serious chest
infection. I recovered from this in January 1990, but continued to suffer
from fatigue and minor illnesses.
,
fitting in my studies around paid work. However, after I had been studying
for just over a year, in December 1989, I developed another serious chest
infection. I recovered from this in January 1990, but continued to suffer
from fatigue and minor illnesses.
med4
Then, in May 1990, when travelling
by train to Liverpool to carry out research for the television documentary
series Breadline Britain in the 1990s![]() ,
I was gradually overcome by intense pain and muscle spasms across my chest
and upper back and down my spine, with the site of the pain appearing to
be just to the right of my spine between my shoulder blades. I also had
general weakness and pins and needles down my right side, arm and leg with
great difficulty in walking as a result of this and the intense pain, and
my neck was very stiff with limited movement, particularly to the left.
This was the onset of the impairment which caused me the greatest difficulty
during the period of my research.
,
I was gradually overcome by intense pain and muscle spasms across my chest
and upper back and down my spine, with the site of the pain appearing to
be just to the right of my spine between my shoulder blades. I also had
general weakness and pins and needles down my right side, arm and leg with
great difficulty in walking as a result of this and the intense pain, and
my neck was very stiff with limited movement, particularly to the left.
This was the onset of the impairment which caused me the greatest difficulty
during the period of my research.
med5
Initially I tried to ignore these symptoms, assuming that
I had trapped a nerve. I alighted at Lime Street station in Liverpool,
and with some difficulty carried out the interviews which I had previously
arranged. Later I did have some concerns that I was experiencing a heart
attack, since I both smoked and had a family history of heart disease![]() ,
but had no idea how to find a hospital. I therefore returned by train to
London, where I collapsed at Euston station. Eventually my partner received
my message that I was ill and collected me by car, by which time I had
decided that I had no real cause for concern, despite the intense pain
and effects on my mobility. Looking back, of course, my judgement was severely
affected by both my condition and my denial of the seriousness of the situation;
my fear of disability was shining through.
,
but had no idea how to find a hospital. I therefore returned by train to
London, where I collapsed at Euston station. Eventually my partner received
my message that I was ill and collected me by car, by which time I had
decided that I had no real cause for concern, despite the intense pain
and effects on my mobility. Looking back, of course, my judgement was severely
affected by both my condition and my denial of the seriousness of the situation;
my fear of disability was shining through.
med6
Another motivation for denying
my pain was the fact that the following day my partner and I were due to
travel to Amsterdam for a long-planned and expensive three-day holiday,
and I was very reluctant to cancel this. Believing that there was no real
cause for concern and the pain would diminish shortly, I therefore left
as arranged. Three more days of agonising pain and disability followed,
and on my return to London I went straight to the accident and emergency
department of my local hospital. By this time I had been informed by the
Amsterdam hotel's masseur that I had a mild scoliosis of the thoracic spine![]() ,
of which I had previously been unaware. However, no X-rays or other tests
were carried out, and the doctor on duty at the hospital diagnosed a pulled
muscle - although he was unable to say which one. He therefore discharged
me after prescribing three days' worth of mild pain killers, and advised
me not to rest or to take any time off work. (Standard advice for back
pain sufferers in the UK is to carry on as normal, with a warning that
rest is counter-productive.)
,
of which I had previously been unaware. However, no X-rays or other tests
were carried out, and the doctor on duty at the hospital diagnosed a pulled
muscle - although he was unable to say which one. He therefore discharged
me after prescribing three days' worth of mild pain killers, and advised
me not to rest or to take any time off work. (Standard advice for back
pain sufferers in the UK is to carry on as normal, with a warning that
rest is counter-productive.)
med7
My own denial of the seriousness of the situation had
now been supported by the medical establishment, but despite this my condition
did not improve. At this point I was not registered with a general practitioner,
since I had complained about the administration of my previous practice,
so I had no-one to whom I could turn for a second opinion. Instead I returned
to work and suffered three more weeks of intense pain and related disability,
before being advised by my employers - who were becoming increasing irritated
by the restrictions which this placed on my activities - to consult an
osteopath. I was fortunate in finding an excellent local practitioner whom
I have seen regularly ever since, and she was able to relieve the acute
pain and related muscle spasms to some extent. After lengthy questioning,
the only cause of my pain and impairment of which we could think was an
incident on the London Underground about a fortnight before my journey
to Liverpool, when I had been crushed by a crowd of drunken stockbrokers
while "strap-hanging" on the way home from work. I had also experienced
a brief faint spell during the night before the journey when the pain came
on. Later, the osteopath felt that the chest infection I had suffered from
five months beforehand was also significant.
med8
Ten weeks after the onset of pain, in August 1990, my
pain had become chronic and I became sufficiently concerned to register
with a male general practitioner. (I would have preferred to see a woman
doctor, but there was none available within the practice.) This doctor
prescribed mild painkillers and referred me back to the local hospital;
I was given an appointment to see a consultant in six months' time, which
was the earliest available. The lengthy waiting period before seeing a
specialist and the GP's lack of concern reinforced my belief that nothing
was seriously wrong, and thanks to the osteopathic treatment, and later
to the regular acupuncture and homeopathy recommended by my osteopath![]() ,
I was able to continue working and to complete my television contract in
October 1990.By this time I believed that the reason why I was still experiencing
severe pain and disability was due to the fact that I had been unable to
rest, and that a week's holiday after finishing the contract would cure
me. (This was the first point when I questioned the medical advice which
I had received at the time of the onset of pain; I now believe that rest
and immediate drug treatment and physiotherapy would have provided my best
chance of recovery.)
,
I was able to continue working and to complete my television contract in
October 1990.By this time I believed that the reason why I was still experiencing
severe pain and disability was due to the fact that I had been unable to
rest, and that a week's holiday after finishing the contract would cure
me. (This was the first point when I questioned the medical advice which
I had received at the time of the onset of pain; I now believe that rest
and immediate drug treatment and physiotherapy would have provided my best
chance of recovery.)
med9
Despite my optimism, the effort of
trying to continue as if my impairment did not exist had left me suffering
from long-term exhaustion, and a holiday followed by several weeks' rest
made little difference. In January 1991 I therefore returned to my general
practitioner to ask if he could refer me for X-rays, bring forward my hospital
appointment and prescribe adequate pain relief in the meantime, since after
seven months I was finding the severe pain very wearing. My GP replied
that he could do nothing about speeding up diagnosis or treatment, but
would in the meantime prescribe better pain relief, although he gave me
no details or advice about the medication involved.
med10
A few days later I felt most peculiar, was unable to sleep
and noticed that the pupils of my eyes were very contracted, while there
had been no effect on my pain. I therefore consulted my acupuncturist,
who confirmed that the medication, Amitriptyline, was in fact a tricyclic
anti-depressant with marked sedative effects, effective only at combatting
the physical symptoms of depression, and that I should have been warned
to avoid alcohol and driving because of the known side-effects. I was extremely
upset by this, but challenging my GP achieved nothing but the advice to
find another doctor if I was unhappy with his treatment. I believe that
the prescription reflected the common tendency within the National Health
Service to treat women as if their problems are psychological rather than
physical, and women's visits to doctors as demands for attention rather
than for treatment.![]() The long-term effects of the drug would also have effectively prevented
me from making further demands.
The long-term effects of the drug would also have effectively prevented
me from making further demands.
med11
I therefore had little choice but to wait for my hospital
appointment, which in the event was brought forward to March 1991. I saw
a male consultant, who prior to examining me locked the consulting room
door "to keep the angry husbands out", and who made a number
of inappropriate comments such as my not needing to worry, since I "had
the body of a twenty year old" (by this time Iwas twenty-nine). He
did not order any X-rays or blood tests, but diagnosed a "slipped
disc"![]() and referred me for physiotherapy. He said he would recommend a course
of exercises, but that the physiotherapists were independent and would
administer the treatment which they thought best. Following this treatment,
he told me, he would administer an anti-inflammatory injection to treat
my "slipped disc" at my next visit. I duly visited the physiotherapy
department, where I was assessed separately by two (male) senior physiotherapists
who decided that exercises would only aggravate my condition. Having tried
traction, which also aggravated my pain, they decided to use ultrasound
and referred me for physiotherapy. He said he would recommend a course
of exercises, but that the physiotherapists were independent and would
administer the treatment which they thought best. Following this treatment,
he told me, he would administer an anti-inflammatory injection to treat
my "slipped disc" at my next visit. I duly visited the physiotherapy
department, where I was assessed separately by two (male) senior physiotherapists
who decided that exercises would only aggravate my condition. Having tried
traction, which also aggravated my pain, they decided to use ultrasound![]() and TNS
and TNS![]() treatment. In all, I made eight visits to the department and this treatment
did appear to be beneficial.
treatment. In all, I made eight visits to the department and this treatment
did appear to be beneficial.
med12
However, when I returned to see the consultant at the
end of April 1991, he became very angry because I had not been given an
exercise regime by the physiotherapists, and said that he "did not
believe in" ultrasound or TNS (the fact that the hospital's administration
clearly did believe in these treatments did not appear to concern him).
I tried to tell him that I had already tried an exercise regime recommended
by my osteopath, as well as taking up Tai Chi in an effort to stop my muscles
from wasting. I had also originally trained as a dancer![]() ,
so both understood the need for and enjoyed exercise, but knew that anything
more than very gentle exercise was making my condition worse. However,
the consultant ignored what I was saying, cancelled my physiotherapy, refused
to administer the promised anti-inflammatory injection and sent me back
to the physiotherapy department for an exercise regime. This the physiotherapists
then refused to give me on the grounds that it was contra-indicated.
,
so both understood the need for and enjoyed exercise, but knew that anything
more than very gentle exercise was making my condition worse. However,
the consultant ignored what I was saying, cancelled my physiotherapy, refused
to administer the promised anti-inflammatory injection and sent me back
to the physiotherapy department for an exercise regime. This the physiotherapists
then refused to give me on the grounds that it was contra-indicated.
med13
At the following appointment I asked again to be X-rayed,
but was refused on the grounds that "nine out of ten bad backs do
not show up on an X-ray, so there is no point". The consultant then
told me that there were no medical conditions with my symptoms (I had written
down my medical history and symptoms for him before my initial appointment,
as is commonly advised); said that if I "thought about it for long
enough [I] would realise that [I] was just depressed"; and discharged
me, walking out of the room while I was still speaking. In retrospect,
I believe that this diagnosis also reflected the common tendency within
the National Health Service to treat women as if their problems are psychological
rather than physical, and women's visits to doctors as demands for attention
rather than treatment.
med14
For the next few months I struggled to uncover the psychological
problem which was causing me such great pain and impairment, since I was
not given a referral to any form of psychiatric service. Nothing obvious
came to mind, particularly given that I had already completed lengthy counselling
in the early 1980s, following the death of my father![]() .
I had tried very hard to maintain a positive mental attitude since becoming
disabled - because I thought that it was essential to a "cure"
- and believed that I had largely succeeded up until this point. Since
the career which I had envisaged had been disrupted, in January 1991 I
had decided to complete my M.A. programme of study at the University of
East London, rather than transferring my registration to PhD as originally
planned. I had also begun working as a media and communications consultant
at the Health Education Authority, since I was unable to continue with
my journalism career and television research
.
I had tried very hard to maintain a positive mental attitude since becoming
disabled - because I thought that it was essential to a "cure"
- and believed that I had largely succeeded up until this point. Since
the career which I had envisaged had been disrupted, in January 1991 I
had decided to complete my M.A. programme of study at the University of
East London, rather than transferring my registration to PhD as originally
planned. I had also begun working as a media and communications consultant
at the Health Education Authority, since I was unable to continue with
my journalism career and television research![]() .
(In the past my work had often involved travelling by public transport,
carrying a shoulder bag, camera bag and briefcase; clearly this was now
impossible.) Although I had to time my work carefully and rest a lot, both
my academic work and paid work were proceeding well, and I did not believe
that this fitted in with a diagnosis of depression. I was also aware that
if I thought about it for long enough, I would become depressed,
particularly since I was still suffering from the effects of long-term
exhaustion.
.
(In the past my work had often involved travelling by public transport,
carrying a shoulder bag, camera bag and briefcase; clearly this was now
impossible.) Although I had to time my work carefully and rest a lot, both
my academic work and paid work were proceeding well, and I did not believe
that this fitted in with a diagnosis of depression. I was also aware that
if I thought about it for long enough, I would become depressed,
particularly since I was still suffering from the effects of long-term
exhaustion.
med15
In retrospect, I am surprised that I gave any credence to the doctor's denial of my problems, since I knew perfectly well that I was suffering from genuine pain and impairment. I also knew that I was not seeking medical treatment as a means of getting attention - as a journalist, writer and politician, I was used to having a large audience, while I have disliked and avoided doctors and hospitals since being hospitalised as a young child. However, we are taught to accept a doctor's opinion as final, apparently to the extent that if a doctor denies that a physical problem exists, we believe them. Susan Sontag also points out that:
part of the denial of death in this culture is a vast
expansion of the category of illness as such.
Illness expands by means of two hypotheses. The first is that every form
of social deviation can be considered an illness . . . The second is that
every illness can be considered psychologically. Illness is interpreted
as, basically, a psychological event, and people are encouraged to believe
that they get sick because they (unconsciously) want to, and that they
can cure themselves by the mobilization of will; that they can choose not
to die of the disease. These two hypotheses are complementary. As the first
seems to relieve guilt, the second reinstates it. Psychological theories
of illness are a powerful means of placing the blame on the ill. Patients
who are instructed that they have, unwittingly, caused their disease are
also being made to feel that they have deserved it.![]()
med16
Fortunately, in January 1991 I had also begun to see a
doctor at the charitable Nature Cure Clinic in West London, on the recommendation
of a friend who is an HIV/Aids activist. Here I was receiving herbal and
homeopathic remedies, together with dietary advice. After trying this regime
for a few months and giving up smoking without noticeable improvement in
my condition, in August 1991 the doctor there questioned me again about
my medical treatment. In particular, he was concerned that no X-rays and
blood tests had been performed. He was unable to refer me for these himself
- the clinic is staffed by doctors from the private Hale Clinic who volunteer
their services - but urged me to see my general practitioner again to obtain
the appropriate referral.
med17
My GP refused, pointing out that I had already seen a
consultant and been diagnosed as suffering from depression, but the doctor
at the Nature Cure Clinic reiterated his advice and arranged for me to
have blood tests performed privately, while my osteopath arranged X-rays
at the National School of Osteopathy in Trafalgar Square. This cost me
several hundred pounds from an income which had been drastically reduced
as a result of my impairment. It also challenged my opposition to private
medical treatment, which I had previously regarded in the light of "queue-jumping"
rather than as an alternative to no treatment at all. As Lisa Cartwright
points out: "Though medicine may control the bodies and communities
it images, it also offers imaging as a class and cultural privilege."![]()
med18
In September 1991 I received the X-ray report, which noted
"degenerative changes suspicious of old, mild osteochondritis"![]() .
Neither the doctor at the Nature Cure Clinic nor my osteopath were certain
of the meaning or significance of this, but since the site of the "osteochondritis"
coincided exactly with that part of my spine which I had always identified
as the site of my problems, it seemed reasonable to assume that a link
existed. I therefore obtained a new general practitioner, this time a woman,
and asked for a referral to a different hospital for a second opinion and
for stronger painkillers in the meantime. After reading a letter from my
osteopath my new GP seemed rather alarmed, saying that "we don't do
the little bones at medical school", but was happy to make the hospital
referral. However, she refused to prescribe stronger pain relief because
of the depression diagnosis (at this point I had been in severe pain for
eighteen months). Later she prescribed non-steroidal anti-inflammatory
tablets (NSAIs) to tackle the cause of the pain, but these left me with
a range of side-effects, including very acid urine which mimicked cystitis,
constant nausea and loss of hearing. I therefore had to abandon the tablets,
after my GP told me that "there is no point in trying other types,
since they are all the same" (fortunately, this assertion eventually
proved to be false).
.
Neither the doctor at the Nature Cure Clinic nor my osteopath were certain
of the meaning or significance of this, but since the site of the "osteochondritis"
coincided exactly with that part of my spine which I had always identified
as the site of my problems, it seemed reasonable to assume that a link
existed. I therefore obtained a new general practitioner, this time a woman,
and asked for a referral to a different hospital for a second opinion and
for stronger painkillers in the meantime. After reading a letter from my
osteopath my new GP seemed rather alarmed, saying that "we don't do
the little bones at medical school", but was happy to make the hospital
referral. However, she refused to prescribe stronger pain relief because
of the depression diagnosis (at this point I had been in severe pain for
eighteen months). Later she prescribed non-steroidal anti-inflammatory
tablets (NSAIs) to tackle the cause of the pain, but these left me with
a range of side-effects, including very acid urine which mimicked cystitis,
constant nausea and loss of hearing. I therefore had to abandon the tablets,
after my GP told me that "there is no point in trying other types,
since they are all the same" (fortunately, this assertion eventually
proved to be false).
med19
In December 1991 - shortly before completing my M.A. -
I received my new hospital appointment. This was not at the Pain Clinic
to which my GP had referred me, since it had now closed due to financial
cutbacks. Instead I was transferred automatically to the Neurology department,
although I was fairly sure that I did not have a neurological problem.
Screening there later found that I had some loss of sensation in my right
side, and nerve irritation which was affecting my right arm, but this was
due to whatever was happening to my back. I was therefore referred on to
the Rheumatology department in June 1992. At this point I was also given
a blood test for cancer. I was fairly sure that I was not suffering from
cancer, since my condition had not progressed. However, I was surprised
not to receive any counselling before the test was administered, since
this is standard practice for HIV and a positive diagnosis would be equally
devastating.
med20
At the time when I was first seen by the Rheumatology
department, my medical notes (later obtained by my solicitor) show that
the original diagnosis of depression was still affecting my treatment,
in conjunction with other assumptions about my role in life as a woman
and my failure to conform. In contrast, despite pointing out to each doctor
I have seen that I am a professional whose career has been severely disrupted
by my impairment, not one mention of this has ever been made in my medical
notes, and the effect on my life has never been seen as relevant.
med21
Rather than making notes about my symptoms as I had presented
them, the rheumatology consultant wrote after my first appointment that
"I found the inter-relationship with the mother a little over-protective
for someone of her age . . ." In fact - although I had left home at
eighteen and my relationship with my mother could not be described as close
- I had taken my mother along to provide my childhood medical history and
because she has three separate nursing qualifications, together with an
Honours degree in Psychology. (I have no reason to suppose that any of
the doctors whom I have seen have qualifications in psychology or psychiatry.)
Perhaps unsurprisingly, the doctor found her to be "somewhat overwhelming
in terms of pressing for a diagnosis and feeling unhappy about previous
management". The notes continued: "I would be quite interested
to interview Miss [sic] Gosling's partner who is apparently now doing most
of the work at home."
med22
It is probable that my very insistence on being viewed
as a professional woman, compounded with my appearance and non-married
status, resulted in my being viewed instead as a dysfunctional woman, whose
refusal to fulfil a traditional role, to "grow up", was my real
illness. In fact, my (male) partner, who attended later appointments, took
an equal share in the housework for many years before I became disabled,
and was always the sole cook. I had no need to "play disabled"
to avoid the washing up; in any case, before I became disabled my income
was sufficient for me to pay for domestic assistance if I had wished. (What
is true is that I had internalised the responsibility for cleaning the
house personally to the extent that I was distressed for a long time after
this ceased to be possible, until the National Back Pain Association liberated
me with the slogan "a little dirt never hurt".) I do wonder,
though, whether my initial treatment would have been different if I had
originally presented myself as someone who wished to get married and to
have a baby, yet was unable to do so as long as I had back pain.
med23
Presumably contact with my partner did convince the rheumatology
consultant that I did have a genuine physical problem, since he eventually
ordered MRI scans![]() and later wrote to my original consultant that "it is difficult to
equate this [diagnosis of depression] with the fact that she has gone back
to study for a PhD and travels down to Canterbury weekly". In April
1993, three years after my problems started, I was finally told that the
scans showed a diagnosis of Scheuermann's Disease or Juvenile Kyphosis
and later wrote to my original consultant that "it is difficult to
equate this [diagnosis of depression] with the fact that she has gone back
to study for a PhD and travels down to Canterbury weekly". In April
1993, three years after my problems started, I was finally told that the
scans showed a diagnosis of Scheuermann's Disease or Juvenile Kyphosis![]() ;
the "osteochondritis" referred to on the original X-ray report
commissioned by my osteopath. In fact, according to my medical records,
this had already been deduced by the Neurology department more than a year
beforehand from the original X-rays, when they had also noted the scoliosis.
This diagnosis had not been told to me, though, since it was "probably
incidental".
;
the "osteochondritis" referred to on the original X-ray report
commissioned by my osteopath. In fact, according to my medical records,
this had already been deduced by the Neurology department more than a year
beforehand from the original X-rays, when they had also noted the scoliosis.
This diagnosis had not been told to me, though, since it was "probably
incidental".
med24
No explanation was given to me when I did eventually receive
the diagnosis, but I was able to find out more from my work as a media
consultant to the Health Education Authority. In non-medical terms, my
upper or thoracic spine is both rounded (kyphosis), giving me round shoulders
and making me appear to have poor posture, and curved to the side (scoliosis),
making my shoulders slightly crooked. As a result the inward curve of my
lower back is also exaggerated, pushing my stomach outwards and my pelvis
back. The curvature is due to the fact that the affected thoracic vertebrae
did not develop properly during adolescence and are wedge-shaped, "malformed".
In fact, the Scheuermann's Disease is clear from looking at myself in the
mirror - particularly after comparing myself with photographs from a book
on "spinal deformities" - but I had never before realised that
my body was not "normal". However, none of the doctors whom I
had seen had noticed, with more than one saying accusingly that I had "very
poor posture".
med25
There is no obvious reason why my spine developed in this
way - there appear to be various and conflicting medical explanations -
but one possible explanation is my allergy to cows' milk products. I have
been taking calcium supplements since discovering this in my early 20s,
and a bone density scan taken in the mid-1990s was normal. However, during
my teenage years I assumed that I was getting all of the calcium which
I needed from milk, and may well have been severely calcium-deficient.
I also fractured my elbow only weeks after the onset of menstruation, which
may well have put my body under severe strain when the bones were growing.
Equally, my mother was told that my brother had just escaped having spina
bifida when he was born, so there may be genetic factors involved.
med26
The diagnosis did explain various things which had occurred
during the later years of my dancing training![]() .
For example, I had been unable to flatten my lower back against the floor
when lying down, could not lift my arms over my head properly or flatten
my back when leaning forward during "centre" exercises, and my
dancing ceased to improve as time went on. However, at the time no-one
told me that my back was different from other students', although it must
have been obvious to my teachers
.
For example, I had been unable to flatten my lower back against the floor
when lying down, could not lift my arms over my head properly or flatten
my back when leaning forward during "centre" exercises, and my
dancing ceased to improve as time went on. However, at the time no-one
told me that my back was different from other students', although it must
have been obvious to my teachers![]() ,
who did not allow me to do much pointe work and who recommended that I
train as a teacher rather than a dancer. Perhaps they did not want to upset
me, but actually the explanation would have been a great comfort, since
I was as competitive as the rest and my failure as a dancer was very distressing.
,
who did not allow me to do much pointe work and who recommended that I
train as a teacher rather than a dancer. Perhaps they did not want to upset
me, but actually the explanation would have been a great comfort, since
I was as competitive as the rest and my failure as a dancer was very distressing.
med27
Another explanation which the diagnosis provided was the
reason why I had developed lower back pain when I was about fifteen, brought
on by dancing. (Significantly, my dancing teacher's first question when
I complained of it was whether it was my upper back which hurt.) From later
reading, it appears that the pain was due to the fact that the area of
the thoracic spine affected by Scheuermann's Disease is rigid rather than
flexible![]() ,
so activities such as dancing or gymnastics which require high degrees
of flexibility can put a strain on the ligaments and muscles of the lower
back as they are required to work harder
,
so activities such as dancing or gymnastics which require high degrees
of flexibility can put a strain on the ligaments and muscles of the lower
back as they are required to work harder![]() .
However, at the time my mother was unable to interest my GP in investigating.
Although my mother was sufficiently concerned to pay for me to see a consultant
privately from a very small income - another example of paying for medical
treatment being the only option, rather than merely the quickest - he only
X-rayed my lower back, which unsurprisingly showed no problems. He did
say that he was surprised that I couldn't lift my legs higher, which perhaps
should have given him a clue
.
However, at the time my mother was unable to interest my GP in investigating.
Although my mother was sufficiently concerned to pay for me to see a consultant
privately from a very small income - another example of paying for medical
treatment being the only option, rather than merely the quickest - he only
X-rayed my lower back, which unsurprisingly showed no problems. He did
say that he was surprised that I couldn't lift my legs higher, which perhaps
should have given him a clue![]() ,
but he discharged me without carrying out further investigations. As I
was discharged, my mother and I both concluded that the pain was insignificant,
again reflecting the tendency to accept a doctor's verdict over the evidence
of our own bodies.
,
but he discharged me without carrying out further investigations. As I
was discharged, my mother and I both concluded that the pain was insignificant,
again reflecting the tendency to accept a doctor's verdict over the evidence
of our own bodies.
med28
If Scheuermann's Disease had been diagnosed during adolescence,
the correct treatment appears to have been to fit me with a spinal brace
until my spine had finished growing, which could have prevented much of
the curvature from developing. (Exercise alone would have been unlikely
to help, since a rigorous ballet training did not prevent the condition
from developing.) I would also have been warned to protect my spine because
of its vulnerability to early degenerative changes: carrying a camera bag,
shoulder bag and briefcase for long distances, together with frenetic typing
in order to meet journalistic deadlines, would not have been recommended.
If I had been diagnosed and treated in adolescence I would probably not
be disabled now, given that the majority of people with mild Scheuermann's
Disease suffer few problems. For more than ten years after I gave up dancing
I had no problems with my back, and degeneration of the affected area![]() of my spine in my twenties and related chronic inflammation, rather than
the Scheuermann's Disease itself, is the cause of my impairment today.
of my spine in my twenties and related chronic inflammation, rather than
the Scheuermann's Disease itself, is the cause of my impairment today.
med29
Following the diagnosis of Scheuermann's
Disease in April 1993, I was advised that the only treatment which could
be offered to me was a course of anti-inflammatory injections, although
I was warned that these might prove to be of little benefit![]() .
The doctor who would administer these injections was, I was told, the consultant
whom I had seen originally in 1991, who also worked at the hospital which
I was now attending. I made it clear that, given my past experience, I
was unhappy about being treated by him, but was told that I must have seen
him "on one of his off-days" and that he was the only option.
Desperate to try anything to relieve my pain - I was now being prescribed
Co-Proxamol (Distalgesic) as pain relief by my GP, after confirmation from
the rheumatologist that I was not suffering from depression, but this was
of only limited benefit - I agreed to see him again.
.
The doctor who would administer these injections was, I was told, the consultant
whom I had seen originally in 1991, who also worked at the hospital which
I was now attending. I made it clear that, given my past experience, I
was unhappy about being treated by him, but was told that I must have seen
him "on one of his off-days" and that he was the only option.
Desperate to try anything to relieve my pain - I was now being prescribed
Co-Proxamol (Distalgesic) as pain relief by my GP, after confirmation from
the rheumatologist that I was not suffering from depression, but this was
of only limited benefit - I agreed to see him again.
med30
The first injection which he administered, in December
1993, was painful but appeared to be of some benefit, although I was concerned
that he did not ask to see the X-rays or scans beforehand and had clearly
not read my notes. When I arrived for the second injection, in February
1994, he rushed to administer it without speaking to me first, so I had
no opportunity to tell him about the pain which I had suffered following
the first injection. I did ask him if he had now looked at my X-rays or
scans, but was told that he was too busy and would look at them instead
during my third visit. Present in the consulting room was a man to whom
I was not introduced, but who was described upon my enquiring as a visiting
GP with an interest in sports medicine. The consultant carried on talking
to this GP, while he administered the injection in a way which was fundamentally
different to the first. He told the GP that "Sclerosin" was marvellous
stuff which you could inject into any joint without doing harm; this surprised
me as I had always understood that great care was needed with anti-inflammatory
injections since they contained steroids. However, by the time that I had
got dressed, the consultant had disappeared.
med31
Following the injection I suffered severe pain which continued
for some weeks. My osteopath was particularly concerned, since she felt
that my reactions did not correspond with an anti-inflammatory injection
although my reactions to the first injection had. On my third visit, in
March 1994, she therefore sent the consultant a letter raising these concerns,
and I also raised them with him myself. His initial response was that I
had had a "normal reaction" to an anti-inflammatory injection;
later, though, as I was undressing, he said that he liked patients to tell
him if he had "injected them in the wrong shoulder or whatever".
He then administered a third injection - still without having seen the
scans or X-rays - which I again understood to be an anti-inflammatory.
However, the consultant subsequently wrote to my
osteopath, explaining that I had been receiving "sclerosant injections
which are mainly sugar and glycerine with local anaesthetic". He advised
her to ignore my complaints of pain, stating that "a lot of the reaction
was psychological": again, I was being accused of attention-seeking
rather than having a genuine physical problem; but again, no psychiatric
help was being offered instead.
med32
I later discovered that sclerosants are used to promote
ligament growth, in order to stabilise loose or hypermobile joints or to
treat pain caused by overstretched ligaments. The part of my spine affected
by Scheuermann's Disease is already rigid, so it is hard to think of a
medical explanation for this treatment (and a search in the Royal Society
of Medicine's library also found none). In any case, it was not the treatment
for which I had been referred or consented to, and increasing an already
stiff area of my spine was likely to cause me further problems. Since,
unknown to the consultant, my osteopath operated an open records policy,
she passed me on the letter. Subsequently, with the support of the National
Union of Journalists and later the Legal Aid Board, I began legal action
for medical negligence.![]()
med33
In the two years following the injections I suffered from
two accidents related to spinal stiffness, although I had had no accidents
at all between 1990, when my impairment developed, and having the injections
in 1994. My pain also increased, and from April 1994 I began taking the
non-steroidal anti-inflammatory (NSAI) drug Naproxen twice daily, which
was effective in reducing the my pain levels without noticeable side-effects.
I discovered that I could tolerate Naproxen, unlike other NSAIs, by chance,
but I have an ongoing concern about the long-term risks of this treatment![]() .
.
med34
I never returned to the hospital where I received the
injections, but some months previously, on the advice of the charitable
Scoliosis Association, I had obtained a referral to the Royal National
Orthopaedic Hospital (RNOH). (Unfortunately, my GP forgot to include the
name of the doctor whom the society recommended in her letter, and I never
saw him). At the RNOH I was first told that the Scheuermann's Disease diagnosis
was wrong, as my spine was not severely enough affected by the osteochondritis
to meet the medical definition, then, after the doctor saw my MRI scans,
the diagnosis was confirmed. I suspect that my posture is actually very
good for someone with Scheuermann's Disease - due to my dancing
training - which masks it somewhat, and in any case the kypho-scoliosis
is itself only mild. But the incident reflects the fact that I was being
classified according to my impairment, and any deviation from their understanding
of it was a fault of mine rather than in their knowledge or approach.
med35
I was then offered a choice of immediate physiotherapy
or a referral to the hospital's Pain Clinic; I could not, I was told, have
both. Since I was told that the immediate physiotherapy would consist only
of recommending an exercise regime before discharging me, I opted for the
Pain Clinic referral. I finally saw a doctor at the Pain Clinic in June
1994, where I was recommended for inpatient treatment in their rehabilitation
unit![]() .
I was told that I would be admitted for three weeks in January 1995, which
would have been ideal timing since I would have recently completed the
PhD research and would be about to start my "writing-up" process.
However, when I wrote to the hospital in January 1995 to ask when I would
be admitted, I was told that the doctor I had seen had had no authority
to give me an admittance date, and I would have to wait for several more
months. I was later offered an admittance date on my thirty-third birthday,
2 May 1995, but my mother had already offered to pay for me to spend ten
days in Florida with her and I decided that a holiday would be of more
benefit. Perhaps this was wise, since my second admittance date, in October
1995, was cancelled by the hospital at forty-eight hours notice. In 1996,
after discussing the treatment further and discovering that, following
cutbacks, it now consisted only of concentrated exercise, I decided that
it was no longer appropriate for me.
.
I was told that I would be admitted for three weeks in January 1995, which
would have been ideal timing since I would have recently completed the
PhD research and would be about to start my "writing-up" process.
However, when I wrote to the hospital in January 1995 to ask when I would
be admitted, I was told that the doctor I had seen had had no authority
to give me an admittance date, and I would have to wait for several more
months. I was later offered an admittance date on my thirty-third birthday,
2 May 1995, but my mother had already offered to pay for me to spend ten
days in Florida with her and I decided that a holiday would be of more
benefit. Perhaps this was wise, since my second admittance date, in October
1995, was cancelled by the hospital at forty-eight hours notice. In 1996,
after discussing the treatment further and discovering that, following
cutbacks, it now consisted only of concentrated exercise, I decided that
it was no longer appropriate for me.
med36
However, the RNOH arranged instead for me to begin physiotherapy
at a local hospital in Cornwall, where I moved temporarily in January 1996.
This began promisingly enough, with two forty-minute assessment sessions
by a senior physiotherapist. Following these, she told me that my current
exercise regime already included all of the exercises which she would have
prescribed, agreed that I was not suffering pain as a result of stiffness
- since the exercises had left me relatively supple - and noted the permanent
muscle spasms around my spine. She then arranged for me to have twice-weekly
hydrotherapy sessions to build up my upper body strength, together with
ultrasound to treat the spinal inflammation. (This was almost five years
after the original ultrasound treatment was cancelled, and six years after
the onset of impairment.) Unfortunately, however, her instructions and
diagnosis were not communicated to the student physiotherapist who was
told to oversee my treatment, and she immediately started me on spinal
mobility exercises. This is the standard treatment for lower back pain;
her actions reflected the facts that the overwhelming majority of back
problems involve the lower back and that patients are defined by their
impairment rather than their individual symptoms.
med37
As I exercised, the combined effects of the buoyancy and
the hot water in the hydrotherapy pool relaxed the protective muscle spasms
around my spine, and the first session left me stiff and in increased pain.
Despite my complaints, though, the student continued the exercise regime
at the next session, and I felt unable to challenge her in case I was denied
treatment. The following morning I woke up with such stiff joints that
I fell over and fractured a toe in my left foot. This left me in increased
pain and unable to exercise or to walk more than a few yards for over a
month - although I still ran a meeting of the Chalet School girls' group![]() in London three days later - but continuing nonetheless with the (now)
correct hydrotherapy exercises did appear to be increasing my muscle strength.
However, within one week of my foot healing the hydrotherapy was abruptly
cancelled, after one member of staff was transferred to another hospital,
the student left for the Easter holidays and the senior hydrotherapist
started working part-time. At the time of writing, over twelve months after
the fall, my toe was still discoloured.
in London three days later - but continuing nonetheless with the (now)
correct hydrotherapy exercises did appear to be increasing my muscle strength.
However, within one week of my foot healing the hydrotherapy was abruptly
cancelled, after one member of staff was transferred to another hospital,
the student left for the Easter holidays and the senior hydrotherapist
started working part-time. At the time of writing, over twelve months after
the fall, my toe was still discoloured.
med38
Fortunately, as a result of the fall
I was prescribed a strong pain-killer, Zydol, by my new Cornish GP, which
was then put on a repeat prescription for me. This was the first time since
becoming disabled that I had received adequate pain relief, since even
after my depression diagnosis was discounted my London GP had refused to
prescribe anything stronger than Distalgesic on the grounds that "no
matter how small the risk, if you became addicted it would be my career
on the line". But with the Naproxen acting as an anti-inflammatory
and with analgesia in the form of Distalgesic and Zydol, I finally had
guaranteed access to effective drug treatment. I am, of course, concerned
about the long-term effects![]() ,
but if a negative choice, it was still the best choice for me.
,
but if a negative choice, it was still the best choice for me.
med39
There are many reasons for the control mechanisms operating
around pain relief, of which the fear of the patient's addiction and the
fear of the professional consequences in that event are important ones.
However, there are also issues of doubt of the patient's pain, suspicion
as to their motives, the belief that the patient should "learn to
live with it", moral objections to interfering with what is often
seen as being imposed by a divinity, and the simple enjoyment of power
over another human being. The mental distress caused by the withholding
of pain relief cannot be underestimated, and ditto the anxiety caused by
not knowing whether pain relief will be forthcoming from one appointment
to another. I believe that everyone has the right to make an informed choice
about their own drug use: they may not always be capable of judging the
effects on their life and health, and this should be monitored professionally
and concerns raised if necessary; but when fully informed, they are in
a far better position than anyone else to judge whether the benefits outweigh
the risks.
med40
Access to drug treatment did not, however, "cure"
me, neither did it negate the effects of my impairment. After more than
six years of disability, the combination of the drug treatment, complementary
therapies, changes to my lifestyle and a regime which included rest, good
nutrition and exercise did have the effect of relieving the worst of my
pain and allowing me to live my life as fully as possible. But I still
suffered from chronic and widespread pain which often made me feel very
unwell and meant that I was easily fatigued; had very limited movement
in my neck; and had problems with my right arm and leg which were exacerbated
by walking. I also continued to lack a detailed diagnosis and specialist
medical care, which medicalisation encouraged me to demand; advice from
the "medical expert" in my negligence action![]() was confusing and later proved to be false.
was confusing and later proved to be false.
med41
Then, in November 1996, I obtained a referral to a consultant
at a Spinal Disorders Unit at a private London hospital, with specialist
experience of treating Scheuermann's Disease. This referral was arranged
via a colleague with contacts in the medical profession and was possible
only because of my own professional contacts; if these contacts had not
existed, it is quite possible that I would never have seen a specialist.
After examining the MRI scans and confirming that my impairment was indeed
due to a degenerative condition arising from Scheuermann's Disease, and
exploring the other steps which I had taken to treat it, the consultant
prescribed a spinal brace for six months. Exercising the affected area
was aggravating the inflammation; immobilising my spine should help to
reduce the inflammation, and thus the pain. Underlining the links between
my experiences as a disabled researcher and my research, I was to wear
the brace until the day I was due to hand in my PhD (my "writing-up"
time had necessarily been extended due to long periods of illness in 1996).
I discuss my experiences of wearing the brace, together with my personal
experiences of disability, on my Home Page web site in My-Not-So-Secret-Life
as a Cyborg.![]()
med42
My experiences as a disabled researcher within the medical
system highlight several points. First, I was not perceived by the medical
profession as a researcher, but rather as a "defective" woman
(no doubt my sexuality also affected this attitude). As a woman I was not
supposed to carry out research or to act on equal terms with men, but to
cook and clean for my husband and to defer to my doctor. Second, the medical
profession did not assign any importance to treating me: because I was
defective, I was undeserving![]() .
Not only was I defective in terms of my femininity and sexuality, I was
also defective because I was impaired. In retrospect it is clear that the
medical profession itself had no difficulty in recognising my condition
as long term, but to tell me this would have been to admit their own limitations.
Instead, the reason why I did not get "better" was given to be
my own psychological defects. As Morris points out: "It is, of course,
less frightening for others to explain our physical differences in terms
of personality inadequacies - it is yet another way of saying that it couldn't
happen to them."
.
Not only was I defective in terms of my femininity and sexuality, I was
also defective because I was impaired. In retrospect it is clear that the
medical profession itself had no difficulty in recognising my condition
as long term, but to tell me this would have been to admit their own limitations.
Instead, the reason why I did not get "better" was given to be
my own psychological defects. As Morris points out: "It is, of course,
less frightening for others to explain our physical differences in terms
of personality inadequacies - it is yet another way of saying that it couldn't
happen to them."![]() By not investigating the nature of my impairment, it was easier to assert
the psychological cause of it. I, on the other hand, continued to believe
in the physical nature of my impairment, and in my right to equal treatment,
including a classification according to the medical model of disability.
By not investigating the nature of my impairment, it was easier to assert
the psychological cause of it. I, on the other hand, continued to believe
in the physical nature of my impairment, and in my right to equal treatment,
including a classification according to the medical model of disability.
med43
Third, the effects of medicalisation profoundly affected
my own attitude to my impairment, and thus to my whole life. For two years
I was unable to see myself as disabled, because I saw my impairment as
a medical and thus "curable" problem. At the least, I therefore
saw myself as "defective" in not being able to obtain appropriate
medical treatment. (Similarly, my mother's grief over the sudden death
of my father had been compounded by her failure to persuade a doctor that
he needed treatment.![]() )
I also did not see myself reflected in stereotypes of disabled people,
and had not yet gained access to images produced by disabled people themselves.
In addition, I did not see myself as having anything in common with the
other disabled people whom I knew, since I had a "medical" problem,
while - in contrast to popular imagery - they appeared to be strong and
in control of their lives.
)
I also did not see myself reflected in stereotypes of disabled people,
and had not yet gained access to images produced by disabled people themselves.
In addition, I did not see myself as having anything in common with the
other disabled people whom I knew, since I had a "medical" problem,
while - in contrast to popular imagery - they appeared to be strong and
in control of their lives.
med44
Morris points out that:
The experience of ageing, of being ill, of being in pain,
of physical and intellectual limitations, are all part of the experience
of living. Fear of all these things, however, means that there is little
cultural representation that creates an understanding of their subjective
reality.![]()
This was extremely isolating, since I therefore experienced my
"treatment" as being due to a personal lack rather than to disabilism.
It also prevented me from accessing the enormous amount of support and strength
which can be drawn from the disability movement. Thanks to the effects of the
disability movement on current thinking in the Labour movement, though, and
to prior contacts with Jenny Morris, Keith Armstrong and Judy Hunt, I experienced
the eventual realisation that I was disabled with huge relief, and embraced
it at once as a potentially positive identity rather than as the personal tragedy
and ultimate blow which society encourages us to believe of it.
med45
Click here to read an update of my condition seven years on.
| Dr Ju Gosling aka ju90's ABNORMAL: How Britain became body dysphoric and the key to a cure is available now for just £3.09 for the Kindle or in a limited-edition hardback with full-colour art plates for £20 inc UK postage and packing. | 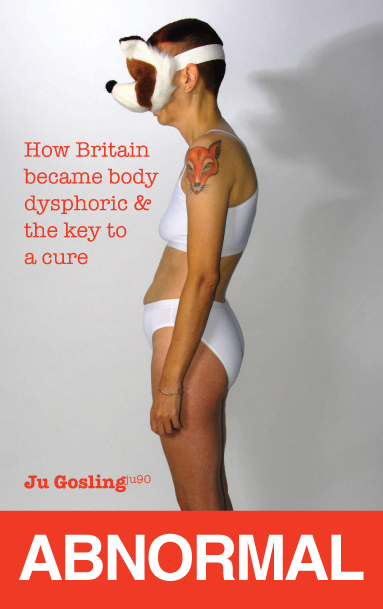 |