Return to: My Experiences as
a Disabled Researcher Index![]()
Return
to: My Not-So-Secret Life as a Cyborg![]()
Return
to: Ju Gosling's Home Page ![]()
I continued to see Mr Crock, head of the Spinal Disorders Unit at the Cromwell Hospital, as a free patient until he retired from private practice as well in 1999, when I was left without a consultant again. By then I had returned to live in London full time, and with the help of a social worker had managed to find an excellent local GP's surgery. Mr Crock had wanted me to undergo a complete rheumatological screening, as well as to have a further MRI scan in order to monitor any changes in my condition since the original scan in 1994. However, although he had recommended that I see a specific consultant at King's College Hospital and my GP had therefore referred me to this doctor, the vagaries of the NHS meant that I saw a locum consultant instead, in autumn 2000.
This consultant, Dr Brown, was helpful in that she identified the onset of my symptoms in May 1990 as being typical of a fracture. Spines affected by Scheuermann's Disease (kypho-scoliosis) are vulnerable to early degeneration, and of course I had already suffered from a number of unexpected fractures in the past. One possible cause of these was the fact that I lack the enzyme to digest cows' milk. This meant that my diet was calcium-deficient until the condition was diagnosed in my early 20s, after which I began to take nutritional supplements and to monitor my diet closely. However, by 2010 it seemed likely that I have a mild genetic collagen disorder too, as I have also developed chronic tendinosis in both hands and wrists and my right shoulder and hip in addition to the ongoing pain around my spine. A collagen disorder would also explain the development of my spinal curvature in the first place, as well as my extreme short sight and astigmatism, and possibly the much longer time it takes my body to rid itself of infection than other people's.
Dr Brown was unhelpful, though, in that she failed to recognise the resulting chronic pain as a medical rather than a psychological condition. She therefore discharged me rather than administering the rheumatological screening and MRI scan that Mr Crock had recommended. (I did not see another consultant until the late noughties, and have still never received the screening or scan.) The friend who accompanied me to the appointment felt that Dr Brown was homophobic - I had begun to live as a lesbian in 1997 - and that this had affected her treatment of me. But it is also true that rheumatology clinics are under enormous pressure, not least from elderly people in need of urgent joint replacements, so there is little time within a burdened National Health Service for treating people with conditions that are benign and largely untreatable.
By the time I saw Dr Brown, I had also become very unwell following a series of discriminatory incidents at a trade union conference in Ireland in April 2000, and this began a round of visits to a series of doctors across London for matters unrelated to my spinal condition. My initial symptoms included hearing loss, loss of visual focus, loss of short-term memory, serious cognitive problems and high blood pressure. I was also collapsing several times a day, when I apparently became very grey and clammy and was unable to function. All I remember was feeling exceptionally unwell, although when my GP came in at the tail end of one attack he found that my pulse was 'dropping off'.
My GP therefore referred me urgently to a cardiologist to discover what effect the illness was having on my heart, but the pressures on the NHS were such that even an emergency appointment took four months to come through. By the time that I was tested at Newham General Hospital, beginning in autumn 2000 and continuing until summer 2001, I was reassured that the illness had left no permanent after-effects on my heart. However, it was too late to tell what the effects had been at the time - or the cause. By summer 2001 the episodes of collapse had also resolved themselves, although I was still prone to becoming unwell very quickly with no warning or apparent trigger, and this has continued.
In contrast, my blood pressure proved intractable to medication. Taking calcium antagonists resulted in the worsening of all of my other symptoms for several weeks, but had no effect on my blood pressure. Taking beta blockers had no side effects, but resulted in my heart being unable to beat fast enough and thus my blood pressure rising instead of lowering. Regular acupuncture was helpful, and eventually my blood pressure simply became unstable instead of permanently high. However, this has left me with other difficulties, since my blood pressure can become very low very quickly, at which time I need help from someone else. (Recognising my symptoms and giving me a drink is effective in stabilising it again, but once my blood pressure is low it is difficult for me to recognise this myself and to take the necessary action without prompting.)
My short-term memory eventually recovered to some extent, and my cognitive problems resolved themselves slowly. I have been left with difficulty in recognising names and faces, and with recalling words, particularly nouns. I also have difficulties with automatic memory 'prompts', although coping strategies allow me to overcome this to some extent. The limited testing that I have undergone has failed to show this, though - tests aimed at the severely brain-damaged and at the full range of IQs are no substitute for appropriate testing, and I have been unable to access this. Instead the tests I had simply showed my IQ varying wildly between tasks, in sharp contrast to the testing carried out by Mensa in the mid-1990s.
My hearing continued to improve slowly, and was first monitored at Newham General Hospital in autumn 2000, when it was found to be at the bottom of the normal range (it had previously been tested as being at the top of the range following an ear infection in the early 1990s). I was left with problems in focusing on sound against background noise and understanding unfamiliar voices. This was eventually diagnosed at the Royal London Hospital as Obscure Auditory Disorder (OAD), and I received training in lipreading and other strategies and techniques which proved very helpful in overcoming this problem to some extent.
My initial visual problems resolved themselves over the first six months, although I was left with pupils that react very slowly to changes in lighting conditions and with poorer fine focus than previously. I was also left with difficulty in processing visual information in strange places, and with a tendency for my brain to fill in what my eyes expected to see in familiar places. This means that I am unable to see things which are not usually in familiar places or which have been moved to unexpected positions, and find it slow to process new environments.
I also discovered from the audiologist that all of these symptoms were linked to the same part of the brain, the lower or 'reptilian' brain. For example, it is a function of the lower brain to focus on sound against background noise, although one would expect this to be an upper brain function. It is also a function of the lower brain to regulate blood pressure. This explains why my personality, creativity and intelligence have been left unaffected by my illness, since these are all functions of the higher brain.
The effects of my illness on my spinal condition have been various. Whereas previously I was able to maintain a high standard of fitness, the illness meant that this was quickly lost, and I have been unable to regain it. This means, for example, that whereas previously I could sit on an ordinary seat with some degree of discomfort, I now need to use my wheelchair outside my home in order to avoid severe back pain when sitting. And whereas I was able to walk well on pavement and other hard surfaces at least some days of most weeks before 2000 - albeit with pain and discomfort - I am now unable to walk more than a few yards outside my home and so rely much more heavily on my wheelchair.
Equally, I am unable to use the spinal brace much because the restrictions that it places on the diaphragm can increase my blood pressure to a dangerous level, and this of course has further affected my mobility. As a result of all this, a bone density scan in 2003 showed that my bone density in my hip was closer to being osteoporotic than to being average, and by 2010 I had osteoporosis.
After being too unwell to work full time for 18 months, I then developed carpal tunnel syndrome within two weeks of returning to full-time work in autumn 2001. This resulted from the ligament around my wrist contracting due to lack of use during my illness, constricting the tendons and nerve. In 2002 I finally received physiotherapy at Newham General Hospital to combat the effects of my illness on my spine and fitness (I had been referred for this by my GP in summer 2000), so this became focused on trying to relieve the carpal tunnel syndrome.
However, by December 2002 my allocated physiotherapy sessions had been used up without significant improvement occurring, and I saw a registrar at the National Hospital for Neurological Diseases who recommended surgery as being the only realistic option left. Unfortunately, after tests had confirmed the carpal tunnel syndrome, I then saw a different registrar (I never did see the consultant I had been referred to originally by my GP). She recommended bracing and waiting to see what happened before discharging me again.
(As with rheumatology departments, NHS neurology departments are full of patients with serious, often life-threatening illnesses; there is no room for treating people with relatively benign conditions. Nonetheless, the first registrar had insisted on testing me for Multiple Sclerosis 'just in case', but as expected the MRI scan for this came back 'entirely normal'. Hopefully the growth of evidence-based medicine will mean that in the future, the treatment which patients receive ceases to vary so much between doctors.)
The physiotherapy department had always warned me against long-term bracing, since it causes permanent restriction of wrist movement. However, I was then left with this as being the only way to avoid permanent nerve damage while waiting for further treatment. My GP re-referred me to the Royal National Orthopaedic Hospital, and when I was eventually seen there in 2003 I was immediately offered surgery. However, with a 14-month waiting list for this, I opted instead for day surgery locally, which I received at the end of May 2004. Although this restored the feeling in my fingers, I soon developed other problems as a result of the tendons thickening, and now have to wear wrist braces full-time on both hands with subsequent limitations on my dexterity.
My GP originally thought that my illness was caused by the discrimination that I had experienced, and it was later confirmed by a senior psychiatrist that the discrimination alone was serious enough to account for an illness of several months' duration. However, when the symptoms failed to resolve themselves as expected, my GP concluded that someone had taken advantage of the discrimination to 'spike' my drink or food. He felt that this would explain my continuing symptoms, either because the spiking involved a 'dirty' street version of a drug, or because a drug had mixed with my medication to form a toxic compound. Obviously, though, it was far too late for testing to prove this theory one way or the other.
I was then referred to the toxicology unit at Guy's Hospital, where the theory was found to be 'plausible', but it was confirmed that it was too late for testing to take place. A neuro-psychologist also confirmed my cognitive problems but concluded that the stress of what had taken place was enough to explain my symptoms, and this has also been the conclusion of other doctors.
However, I received lengthy counselling from an NHS specialist psychotherapist in order to cope with the effects of my illness on my life, and she concluded that I showed no signs of having mental health problems, nor of having had these in the past. I also underwent testing for anxiety and depression on several occasions for four years after the onset, and always scored within the normal range. Any psychiatric condition is therefore causing a chemical imbalance in my brain, or caused a pemanent lower brain injury at the time, rather than producing treatable mental health symptoms.
In the resulting Tribunal, the NHS itself was blamed for the permanent impairments that have resulted. The same senior psychiatrist who concluded that the discrimination I experienced was enough on its own to cause a serious illness of several months' duration, also concluded that the continuing symptoms could be explained by the shock caused to me by my GP's diagnosis of 'poisoning'. I find this unlikely, since the 'spiking' theory provided me with a common and easily understandable external cause for my illness rather than being an ongoing cause of concern. Unfortunately women, and particularly disabled women, are still stereotyped as being nervous, if not hysterical, in the extreme, while homosexuality is commonly seen as a psychiatric symptom in itself.
In my opinion, if my GP was mistaken as the Tribunal concluded, then either the psychiatric injury was permanent from the start, or the stress of the legal case which arose from the discrimination was responsible for it becoming permanent, particularly as the case dragged on for more than four years. The refusal of my union to accept or take any responsibility for the discrimination and to apologise was far more deeply hurtful and upsetting than the chance actions of a stranger ever could be. Equally, the knowledge that my own union rather than a stranger was responsible for a serious illness was much harder to come to terms with.
It may be that, in the future, I obtain a greater understanding of all of my experiences within the medical system. In the meantime, I have learned over the years that the cause is less important than the effects, and that getting on with life regardless is more important than all of these.
Return to: My Experiences as
a Disabled Researcher Index![]()
Return
to: My Not-So-Secret Life as a Cyborg![]()
Return
to: Ju Gosling's Home Page ![]()
| Dr Ju Gosling aka ju90's ABNORMAL: How Britain became body dysphoric and the key to a cure is available now for just £3.09 for the Kindle or in a limited-edition hardback with full-colour art plates for £20 inc UK postage and packing. | 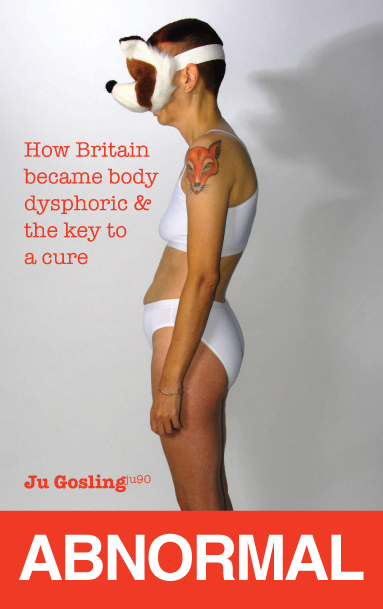 |